In this blog I’m going to be covering two topics that I have gained further insight to via my trauma therapy group; trauma stacking and the trauma tree. I have decided to conduct more detailed research and share my anecdotes also.
We have already discussed the ACE Study and I have mentioned that I have the diagnosis of CPTSD so the relevance right now is high for me.
The below studies are based on trauma in general, which can be extremely diverse, not just the 8 initial ACEs.
A study conducted, shows that those with childhood traumas are more likely to develop PTSD and CPTSD and as an adult, when facing traumatic events, have more complicated responses due to this, generally presenting in a heightened and more prominent state. This is linked to the HPA axis changes (too medical for my liking at this stage, but in very basic terms, a key component in the body’s stress response system) which heighten vulnerability to further traumas in later stages in life. Based on another study from the APA, patients with CPTSD are already prone to re-traumatisation due to hypervigilance, a main trait in PTSD and CPTSD.

Hypervigilance is increased alertness, linked to the anxiety in PTSD/CPTSD and for me, usually presents as being very easily overstimulated and having quick outbursts because of it, often like a dog attempting to yap at your hand that’s trying to take away its food. The difference is that I’m the one biting my own hand here.
It also presents as troubles sleeping, constantly having very vivid nightmares about past traumatic events which as we all know, if you’re not getting a good nights sleep, you’re already starting the day off on a bad foot. This doesn’t necessarily make me tired and I think I function well on little sleep, it’s what’s happening in my sleep…
I love a good gory horror movie and don’t get scared easily. Bugs? no problem. Ghost stories, paranormal activity? fine with me. But imagine watching everything bad that’s ever happened to you/loved ones from what feels like a glass cage, you are completely powerless and see it all reoccur, over and over again, night after night for what seems like the entire duration of your sleep… It can get a bit disrupting, regardless of if you’re yawning or not.
Now, after what seems to be the longest intro ever, lets get into things…
Trauma Stacking

Trauma stacking, again, put basically, as in the name, is multiple traumatic events happening over a long period of time to an individual. Due to previously disrupted coping mechanisms and vulnerability due to the PTSD/CPTSD the individual has, new traumas are often much harder to experience.
Anecdotally, every time I experience a traumatic event, I feel worse than the previous time, with my most recent traumatic episode requiring the most medical intervention I have needed in my life. Currently, I’m getting slightly better, I’m working on myself a lot, but I’m scared to get back up off the ground. Being closer to the ground seems to be less scary. They do say, the taller the mountain, the longer the fall, or something along those lines – I think..?
With each event being worse than the last, I’m never sure if I could go through it again.
I visualise trauma stacking as Jenga, and it’s only a matter of time until the tower falls, despite how many times it’s been repaired and the holes filled, so although trauma can be deemed inevitable, it’s important to understand the difficulties and differences people may face when experiencing a traumatic event. Someone may have only had one piece placed on them yet, whilst another has got 8 blocks hanging on a single piece… Compassion is key.
Biomed Central has found that CPTSD patients often have an earlier onset response to traumatic situations as well as find trauma inflicted by someone familiar. They are also are found to have more than 2 accompanying mental health conditions alongside CPTSD. This makes it difficult to treat for multiple reasons. As mentioned, we know that there is currently no medication specifically targeted for PTSD or CPTSD, and with additional mental health conditions it’s very likely that multiple options are going to have to be attempted before finding a successful combination that can also assist with the PTSD/CPTSD symptoms the patient is struggling with.
Since the 26th of July I have tried 5 medications and I am currently still in my first week of a new mixture of 4 of these medications. The difficulties the healthcare professionals have had is not being able to treat my CPTSD without further alleviating symptoms of my depression and/or anxiety with the mood stabilisers, PRN medication, anti-depressants and sleeping aids so anecdotally, I have felt the effects of this first hand.
The Trauma Tree
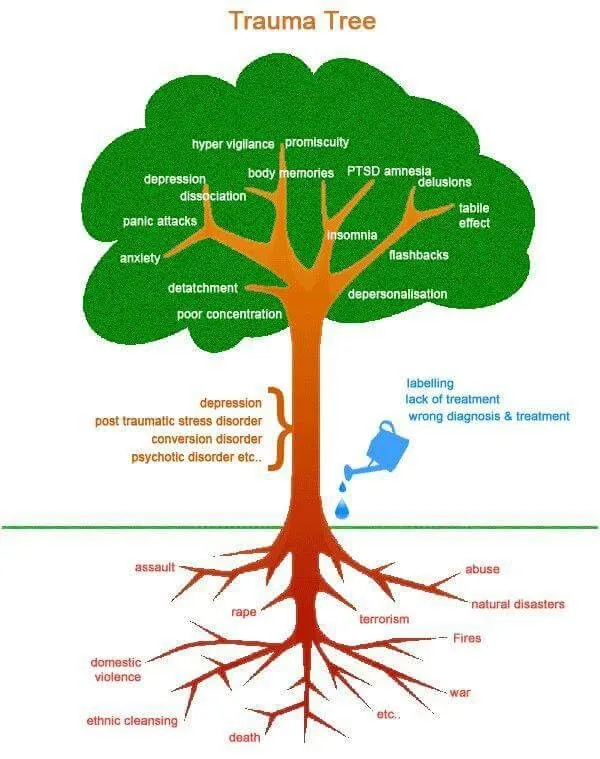
Below I have attached a photo that represents the trauma tree. Each traumatic event represents a root, with the body of the tree becoming mental health disorders such as depression, anxiety, PTSD, Bipolar… The branches/leaves of the tree will then represent a response based on these such as panic attacks, hypervigilance, isolation, panic attacks, poor concentration and promiscuity just to name a few. For me, when viewing this alongside the ACE study and the tendencies for individuals with high ACE scores and the related harmful behaviour/health issues of the percentages rising, the link is quite clear.
Mental health services will not work until screening services are more comprehensive, until patients are listened to further, until we have a more accepting and compassionate social environment, until healthcare is viewed holistically.
I always invalidated my traumas until the past year or two but since becoming more aware of mental health, I have been able to notice that even leaving one symptom untreated can cause failure of treatment in the remaining conditions. With over 50 years of information on PTSD, why is there no medication specifically targeted for it yet, why is it not mentioned more frequently, why are traumas still stigmatised and belittled, why are traumas seen as shameful?
There is much we need to do to improve the care, and it starts with education and empathy.
Sources
CDC The ACE Study
