
Six months ago, if you had asked me about therapy, I would have told you it was useless. After years of trying everything from private counseling to CBT (Cognitive Behavioral Therapy) and DBT (Dialectical Behavioral Therapy), I had grown frustrated and skeptical. Medication was my lifeline, the one thing I believed kept me functioning. I was convinced that pharmaceuticals were my only option and that I would never be able to live without them. To some degree, I still believe I’ll need medication for the rest of my life, and I remain reliant on it. However, something shifted after an intense seven-day therapy session during a stay in a crisis house.
At the time, I didn’t realise how much the therapies I’d participated in over the years had quietly influenced me. Now, as I reflect on the experience, I’ve noticed a significant change in myself. Mental health professionals have often told me that I’m “resourceful and self-aware,” which I’ve come to see as both a blessing and a curse. While self-awareness can be empowering, it can also be overwhelming when paired with the inability to regulate emotions. Therapy has helped me articulate my needs, communicate better with professionals, and truly understand the complexities of my emotions. I’ve learned that while I understand my feelings, I struggle with managing and controlling my response to them. Despite the challenges, I feel more in control of my mental health than ever before, and that’s an incredible feeling.
For many years, I put medication on a pedestal, seeing it as the only way I could maintain stability. Therapy was an afterthought, something I viewed as ineffective. But through my journey, I’ve come to understand that while medication is essential for keeping me stable on a day-to-day basis, therapy offers a much wider picture. Therapy allows me to process the past and heal for the future, while medication provides the stability I need to function in the present.
Finding Balance: Medication and Therapy
I do believe that medication will remain a lifelong part of my treatment, but it should not be the only option, nor the only step for people seeking help. Mental health services are often too quick to discharge patients with no follow-up and too slow to provide adequate support. This experience leaves people feeling isolated and neglected, which only worsens their mental health. A more balanced approach is needed—one where therapy and medication are offered together from the beginning, without requiring people to jump through hoops, as I’ve said before, to prove they are ‘ill enough’ to deserve a more holistic approach.
The Power of Self-Care and Distraction Techniques
One positive outcome of therapy has been learning effective distraction techniques. For a long time, I felt professionals underestimated the difficulty of completing even simple tasks during a depressive episode. They might suggest something like “write down 20 things you’re grateful for” or “name five things that start with S”—activities that seem easy to someone in a stable state but are completely overwhelming when you’re struggling to do the most basic tasks many others don’t even think of, such as eating that day, or brushing ones hair. However, I’ve learned that distraction techniques can be powerful when used at the right time—for me these rarely work when in moments of crisis but rather when in a more stable state, aiding relapse into depressive episodes once again.
For me, self-care has now become a daily ritual. I’ve gone 44 days of completing multiple self-care steps, which can be as simple as drinking a glass of water or as involved as painting a room. It now feels strange when I go more than a few hours without doing something that supports my well-being. This, too, has come from therapy, not medication.
Opening Up to Holistic Approaches
Another crucial change in my mindset has been growing more open to holistic approaches to healthcare. The more I’ve reflected on my mental health journey, the more I realise that mental health services are often too rigid. Discharging patients too quickly, focusing solely on medication or short-term therapy, and overlooking alternative treatments creates unnecessary barriers for those seeking long-term stability.
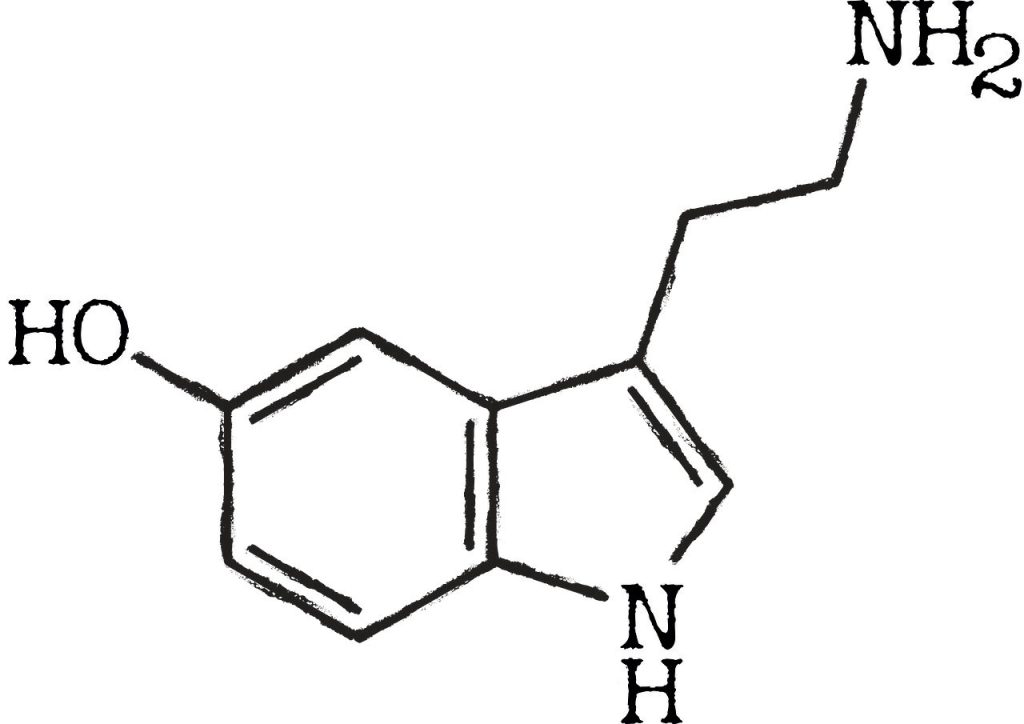
I believe that support should be more integrated into everyday life, whether that’s through regular mental health check-ins at workplaces or accessible community programs where support is provided in more options than a leaflet with helplines on, where there are people to speak to, where finding a professional doesn’t feel like trying to find a needle in a hay stack! Mental health surveys, for example, could help employers better understand the needs of their staff, or ‘mental health centres’ similar to GP surgeries need to be opened. Further research and data collection are crucial, as is communication between healthcare services. The government, the NHS, need to be open to alternative treatments, including those that are currently under-researched or controversial, such as cannabis-based medicines (CBMPs), esketamine, and transcranial direct current stimulation (TDCS). These treatments show promise and could be life-changing for many, but they are often inaccessible or dismissed due to stigma or a lack of investment in research.
In conclusion, my journey has taught me that mental health care must be multifaceted. Medication can stabilise, but therapy is essential for healing, growth, and long-term recovery. Holistic approaches offer even more possibilities, challenging the conventional methods that often leave people feeling underserved or dismissed. Moving forward, mental health services need to evolve—support should be continuous, personalised, and accessible to everyone without unnecessary barriers. By embracing alternative treatments, promoting mental health awareness in everyday life, and rethinking how care is provided, we can create a system that truly meets the needs of all individuals.
